Clinical trials generate large, high-stakes datasets used to determine whether a treatment is safe, effective, and ready for approval. Knowing how to analyze clinical trial data: methods, tools, examples is essential for turning raw patient and study records into statistically valid, audit-ready results. Weak or inconsistent analysis can lead to biased findings, regulatory rejection, and expensive delays.
Clinical trial data analysis follows a controlled framework that includes predefined endpoints, validated statistical techniques, compliant data handling, and transparent reporting. Analysts evaluate outcomes, adverse events, subgroup effects, and repeated measurements over time while preserving traceability and reproducibility throughout the workflow.
This guide explains how to analyze clinical trial data step by step, covering core methods, practical tools, worked examples, visualization, dashboards, and topline interpretation. If you need expert support with regulated statistical workflows and modeling, Professional biostatistics help can support your study analysis and reporting.
Understanding Clinical Trial Data Analysis
Clinical trial data analysis is the process of transforming collected trial data into statistically valid findings about safety, efficacy, and treatment effect. Data typically comes from electronic data capture systems, laboratory systems, patient reported outcomes, imaging results, and monitoring devices.
Before modeling begins, datasets must be validated and structured according to protocol definitions and regulatory standards. Analysts work with endpoints, covariates, treatment arms, and time-to-event measures. Common model families include regression models, survival models, mixed models, and repeated measures analysis.
Accuracy, traceability, and reproducibility are core requirements. Regulatory reviewers expect transparent analytical logic, documented assumptions, and validated outputs.
How to Analyze Clinical Trial Data Step by Step
A reliable clinical trial analytics workflow follows a defined sequence so results remain valid and defensible.
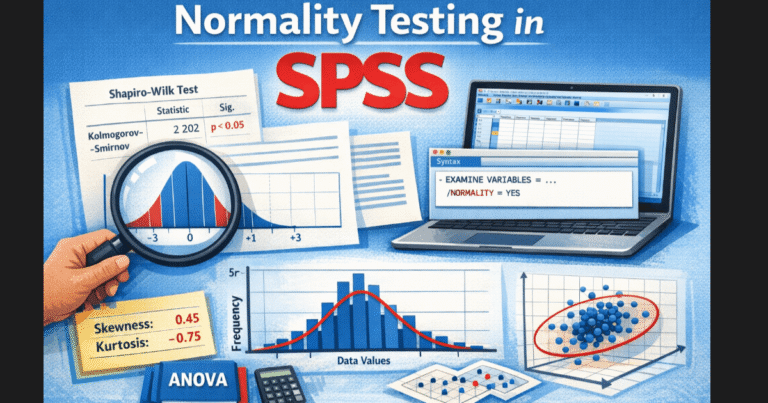
First, analysts perform data cleaning and validation. This includes range checks, duplicate detection, protocol deviation flags, missing value handling, and consistency checks across sites. Clean data reduces bias and model instability.
Next comes descriptive analysis. Baseline characteristics, enrollment distribution, adherence rates, and outcome distributions are summarized using tables and summary statistics. This establishes population comparability across treatment arms.
Inferential analysis follows. Statistical tests and models evaluate whether treatment effects differ significantly between groups. Depending on design, this may include ANOVA, logistic regression, Cox proportional hazards models, or mixed effects models.
Subgroup analysis is then conducted to examine treatment performance across demographic or clinical strata. Analysts must predefine subgroup logic to avoid post-hoc bias.
Safety and efficacy evaluation runs in parallel. Adverse events, severity grades, and exposure adjusted rates are compared between arms.
Finally, results are packaged into statistical reports, tables, and visual outputs suitable for regulatory and stakeholder review.
Get Expert Help With Clinical Trial Data Analysis
Stuck with your clinical or research dataset? We handle cleaning, modeling, testing, and interpretation for student projects.
✓ Confidential handling ✓ Academic-grade reporting ✓ Fast turnaround ✓ Student-friendly pricing
Statistical Methods Used in Clinical Trial Data Analysis
Statistical analysis of clinical trial data depends on study design and endpoint type. Continuous endpoints often use linear models or mixed models. Binary endpoints rely on logistic regression or chi square testing. Time-to-event endpoints use survival analysis methods such as Kaplan Meier curves and Cox models.
Repeated measures designs require longitudinal modeling approaches that account for correlation within subjects. Noninferiority and equivalence trials require specialized hypothesis frameworks and margin definitions.
Multiplicity adjustment is applied when multiple endpoints or comparisons exist. Sensitivity analyses test robustness under alternate assumptions. Power calculations and effect size interpretation are essential for proper conclusion framing.
Method selection must match protocol definitions and statistical analysis plans.
Clinical Trial Analytics Tools and Software
Modern clinical trial analytics relies on specialized statistical software. SPSS supports structured modeling, regression analysis, survival analysis, and reporting workflows suitable for regulated environments. R provides flexible modeling, reproducible scripts, and advanced visualization capabilities. Python supports machine learning, automation, and data integration pipelines.
Analysts often combine tools. For example, data preparation in Python, modeling in R, and reporting in SPSS. Tool choice depends on sponsor standards, audit requirements, and analyst expertise.
Using validated scripts and version-controlled code improves reproducibility and regulatory confidence.
If your team lacks in-house statistical capacity, myspsshelp.com provides clinical and survey data analysis support using SPSS, R, and Python workflows.
Clinical Trial Data Visualization and Dashboards
Clinical trial data visualization improves interpretation speed and decision quality. Visualization converts dense tables into interpretable patterns for investigators and sponsors.
Common visuals include survival curves, forest plots, adverse event heatmaps, enrollment curves, and endpoint distribution charts. Visualization also supports anomaly detection and site performance monitoring.
Clinical trial dashboards combine multiple metrics into real-time monitoring panels. Dashboards track recruitment, retention, protocol deviations, and safety signals across sites. Interactive dashboards support faster operational decisions.
Tools commonly used include Power BI, Tableau, and statistical software visualization modules. Clear visuals also improve regulatory submission clarity.
What Is Topline Data in Clinical Trials
Topline data in clinical trials refers to early summary results released soon after database lock. These results focus on primary endpoints and major safety indicators without full subgroup or secondary endpoint detail. Topline results help sponsors and investors understand trial direction quickly. However, topline data should be interpreted cautiously because deeper analyses may later modify conclusions.
A strong clinical trial data analysis workflow separates topline summaries from final validated analyses. Analysts document differences between preliminary and final outputs to maintain transparency. Including a topline analysis plan before trial completion improves reporting discipline.
Clinical Trial Data Analysis Example Workflow
Consider a randomized two-arm drug trial with a time-to-event endpoint. After database lock, analysts validate subject records and confirm endpoint definitions. Baseline comparability is checked using descriptive statistics.
A Kaplan Meier survival curve is produced for each arm. A Cox regression model estimates hazard ratios while adjusting for covariates. Sensitivity analysis tests alternate censoring rules. Subgroup analysis evaluates treatment effect across age groups.
Results are visualized using survival plots and forest plots. Outputs are compiled into statistical tables and reviewer-ready summaries.
This structured workflow reduces analytical risk and improves audit readiness.
How to Interpret Clinical Trial Data Correctly
Interpretation requires more than statistical significance. Analysts evaluate effect size, confidence intervals, clinical relevance, and consistency across analyses. A statistically significant result with minimal effect size may lack practical value.
Interpretation also considers study power, protocol adherence, and confounding risk. Analysts verify whether findings generalize beyond the sample population.
Regulatory interpretation combines statistical outputs with clinical judgment and safety context. Balanced interpretation prevents overstated conclusions.
Clinical Trial Data Analysis Support Using SPSS, R, STATA, Jamovi & Python
Professional statistical analysis for theses, dissertations, and clinical research datasets using industry-standard tools.
✓ Multi-software expertise ✓ Reproducible results ✓ Methods explained clearly ✓ Secure data workflow
How to Access Clinical Trial Data
Researchers looking to analyze clinical trial data can access public registries and sponsor data portals. Clinical trial registries publish structured trial summaries and selected datasets. Some sponsors provide controlled access through data request programs.
Access requires privacy safeguards and approved research proposals. Standardized data formats improve reuse and secondary analysis opportunities.
Open data initiatives continue to expand collaborative research possibilities.
Get Expert Help With Clinical Trial Data Analysis
Clinical trial datasets are complex and high risk. Errors in modeling, interpretation, or reporting can delay approvals and damage credibility. Professional statistical support improves accuracy and compliance.
myspsshelp.com provides expert clinical and research data analysis using SPSS, R, STATA, Excel, Jamovi and Python among others. Support includes statistical modeling, visualization, dashboard creation, and regulator-ready reporting.